I am currently an adjunct professor at the University of Maryland’s Fischell Department of Bioengineering.
Redesigning Healthcare was a series of experiential learning classes I co-designed and co-instructed with clinicians at Stanford’s d.school between 2013 and 2020.
How I teach:
Past Topics
-
Co-taught with Dr. William Rhine, Head of Neonatology at Lucile Packard Children’s Hospital. The hospital L&D experience became a backdrop for learning design thinking methodology. Our approach was to give students the opportunity to develop empathy for mothers, partners, babies, and clinicians in labor and delivery through observing simulations, synthesizing research, and developing novel products and protocols to improve care.
-
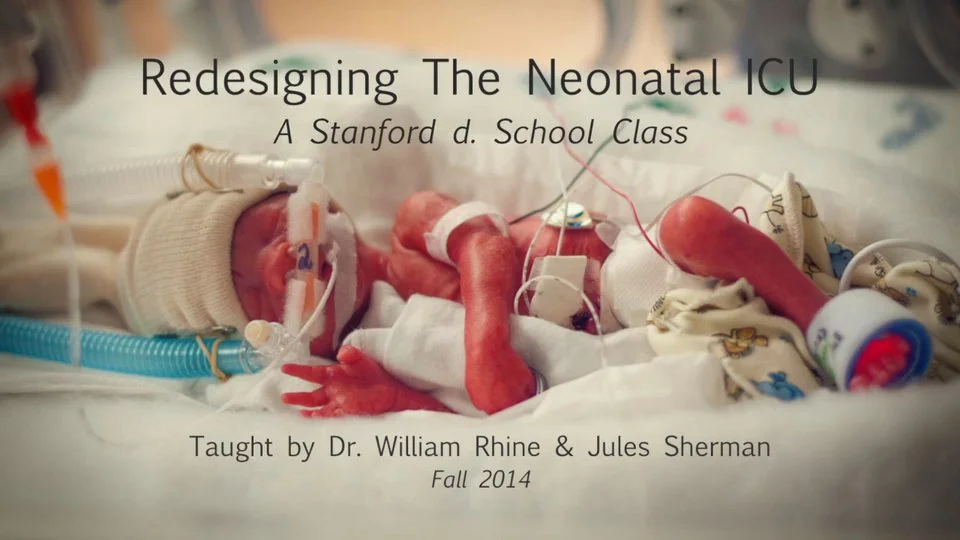
Co-taught with Dr. William Rhine, Head of Neonatology at Lucile Packard Children’s Hospital. Redesigning the Neonatal ICU informed students about current challenges in the NICU environment through expert speakers, literature, CAPE simulations, and field trips. Simultaneously, we studied the users: their environment, their behavior, and emotions. Students developed innovative products and applications to improve care and communication between clinicians and parents.
-
Co-taught with Dr. Henry Lee. This class was inspired by research I am currently participating in regarding how to improve safety in labor and delivery, funded by an AHRQ grant. Dr. Henry Lee, and I informed students about challenges in the L&D environment through direct observation in a simulated environment and the hospital. Simultaneously, we studied the users: their environment, protocols, communication and behavior. Students developed innovative products and applications to improve safety and healthcare outcomes.
-
Co-taught with Dr. Henry C. Lee, Seamus Harte, and Hamsika Chandrasekar. This class was for Stanford medical students to experience the challenges patients with chronic disease face day-to-day through direct observation, and then communicate their insights through storytelling techniques.
-
Co-taught with Dr. Nicole Yamada, Dr. Henry Lee, Dr. Ruth Ann Crystal and Dr. Janene Fuerch. Students observed two neonatal and obstetric medical procedures (infant intubation and maternal hemorrhage protocol), then analyzed the scenarios by watching the simulation videos with our clinicians. Students also interviewed the clinicians about these procedures using field guides they created. Information was synthesized, and students presented their user, the clinical problems they identified, and an innovation/new vision. Students groups presented their work to a panel of designers and clinical experts. This multi-day workshop was held at The Center For Advanced Pediatric & Perinatal Education.
-
Co-taught with Dr. Nicole Yamada, Dr. Henry Lee, Dr. Ruth Ann Crystal and Dr. Janene Fuerch. Students observed and learned (hands-on) how to perform two neonatal and obstetric medical procedures (infant intubation and maternal hemorrhage protocol), then analyzed the scenarios by watching the simulation videos with our clinicians. Students also interviewed the clinicians about these procedures using field guides they created. Information was synthesized, and students presented their user, the clinical problems they identified, and an innovation/new vision. Students groups presented their work to a panel of designers and clinical experts. This multi-day workshop was held at The Center For Advanced Pediatric & Perinatal Education.
-
Co-taught with Dr. Lee Sanders, Chief of General Pediatrics, Stanford. In this class, our aim was to imagine novel interventions that could reduce health disparities for children with medical complexity (CMC). Students designed products and services that aimed to improve care among low-resource patients and their families.
-
Co-taught with Dr. Henry Lee, Neonatologist. In this class we focused on the pediatric population who have feeding challenges in the neonatal ICU, the labor and delivery room, and at home once discharged. Students designed novel medical devices to improve care for children struggling with various feeding challenges.
-
Co-taught with Dr. Lee Sanders, Chief of General Pediatrics, Stanford. In this class, our aim was to imagine novel interventions that could reduce health disparities for children with medical complexity (CMC). Students designed products and services that aimed to improve care among low-resource patients and their families.
-
Co-taught with Dr. Lee Sanders, Chief of General Pediatrics, Stanford. Telehealthcare has found itself at a point of remarkable growth and change due to the COVID-19 pandemic. Our class asked students to consider what aspects of telehealth are most efficacious and then challenged them to design solutions to ensure equitable delivery of care among marginalized groups impacted by systemic racism. Students identified healthcare disparities with stakeholders from underserved communities and prototyped innovative technology-based service designs to address the digital divide.
Class Videos:
Redesigning The Neonatal ICU
Redesigning the Neonatal ICU informed students about challenges in the NICU environment through expert speakers, literature, medical simulations, and field trips. Simultaneously, we study the users: their environment, their behavior, and their emotions. Our goal was to identify needs that could lead to product, system or service innovation and will improve safety and quality of care.
Design for Child Health Equity
In this class, our aim was to imagine novel interventions that may reduce health disparities for children with medical complexity (CMC). Students designed products or services with potential to be helpful for this population of patients and their families.
Use, Usability & Meaning: A Design-Thinking Approach to Simulation Learning
The idea for this class started with my question: Does hands-on immersion yield deeper insights? The resounding answer is "yes," as engaging all senses fosters heightened understanding and innovation. These transformative classes were held at the Center for Advanced Pediatric & Perinatal Education (CAPE) and supported by the Agency for Healthcare Research and Quality and Stanford’s d.school.
Designing For Safety In Labor & Delivery
Designing For Safety In Labor & Delivery was inspired by my own hospital birth experience and the research I conducted with an interdisciplinary team at The Safety Learning Lab For Neonatal & Maternal Care at Stanford Medicine.
Design for Pediatric Feeding Challenges
Our two-quarter class, Design For Pediatric Feeding Challenges, focused on the pediatric population who have feeding challenges in the neonatal ICU, the labor and delivery room, and at home once discharged. Our aim was to teach design thinking methodology as a pathway for healthcare product design. Students learned the Stanford BioDesign method for needs prioritization, and storytelling techniques.
What students have to say: