Tracheostomy Care Research
Equitable Care for Children With a Tracheostomy: Addressing Challenges and Seeking Systemic Solutions
Abstract
Children with medical complexity (CMC) often face significant barriers to accessing care, obtaining appropriate insurance coverage for medical devices, technology, supplies, home nursing and social services. These challenges, when viewed through the lens of social determinants of health, highlight concerns about healthcare inequity. These inequities can impact CMC by limiting access to follow-up appointments, leading to disproportionate use of emergency department services, restricting support services, reducing the quality of medical products and increasing the likelihood of adverse events. Addressing these concerns requires comprehensive policy changes at both state and federal levels. Using exploratory thematic analysis, we identified challenges and opportunities for improvement regarding (a) access to health insurance, (b) procurement of essential medical supplies, (c) logistical constraints and (d) identifying interim solutions.
“100 Things I Wish Someone Would Have Told Me”: Everyday Challenges Parents Face While Caring for Their Children With a Tracheostomy
Abstract
Equitable access to appropriate care, emergency department services, and in-home support aids are needed to minimize the occurrences of adverse events that have a significant impact on families. However, many families of children with medical complexity (CMC) lack consistent care due to issues of health inequity. We conducted 11 qualitative interviews with primary caregivers who were asked about their experiences of providing care to children who have a tracheostomy and are supported by multiple life-saving machines at home. Guided by ecological systems theory, we identified three themes that contextualize the lived experiences of the participants who expressed needs that arose from poor interactions within the mesosystem. Findings convey participant frustrations that result from insufficient support, ineffective training, and inadequate healthcare coverage.
Tracheostomy Tube Monitoring Accessory to Detect Accidental Decannulation and Obstruction Emergencies in Ventilator-Independent Pediatric Patients
Abstract
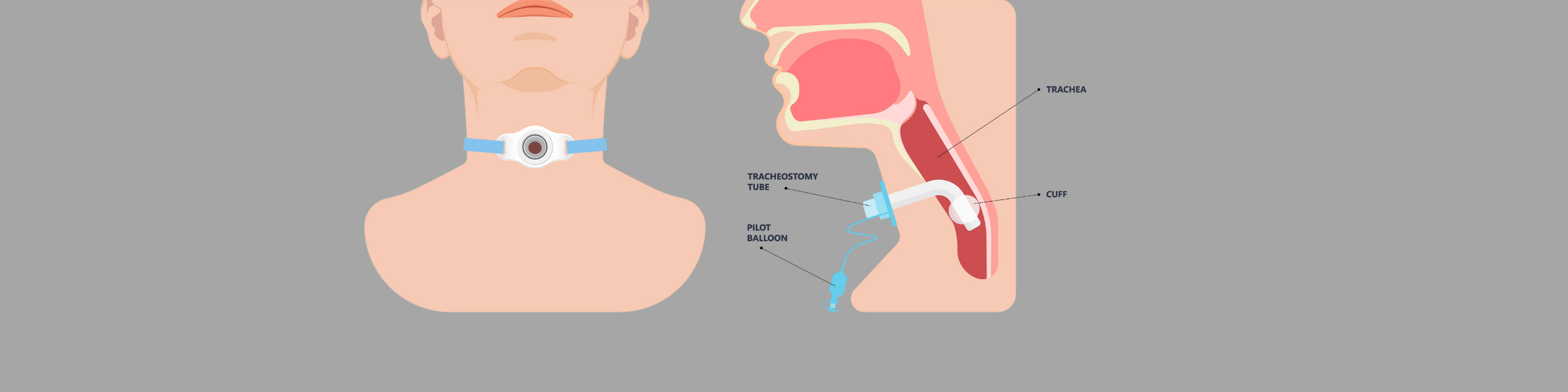
Introduction: Some of the leading causes of tracheostomy-related complications in pediatric populations are accidental decannulation and obstruction events that result in permanent neurological damage or death if not mitigated quickly enough. Despite the severity of tracheostomy tube emergency events, there is currently no effective medical technology available that can specifically detect accidental decannulation or obstruction in a tracheostomized patient that is not ventilator dependent. Therefore, a pediatric tracheal breathing model system was developed to assist with testing new tracheostomy tube technologies for identifying emergency events.
Methods: A custom carbon dioxide monitoring tracheostomy tube attachment was engineered to collect breathing waveform data during emergency events (e.g., improper insertion, accidental decannulation, and mucus obstruction). Anatomically accurate pediatric tracheal models for various age groups (0-3 months, 2-4 years, and 10-12 years old) were developed with modeling software and a 3D printer. A breathing simulator was integrated with the tracheal models to generate age-dependent respiration patterns during simulated tracheostomy tube emergencies.
Results: Carbon dioxide readings from the custom tracheostomy tube attachment indicated distinct waveform recordings during simulated tracheostomy tube emergency events for all age groups tested. During incorrect insertion, accidental decannulation, and complete blockage of a tracheostomy tube, exhaled carbon dioxide readings remained static at ambient levels. Partial mucus obstruction of a tracheostomy tube decreased exhaled carbon dioxide waveform amplitude relative to unobstructed conditions.
Conclusions: The tracheostomy tube attachment successfully recorded respiration patterns during simulated tracheostomy tube emergencies in pediatric patients of varying age. Breathing waveform data collected from the model system will aid in the development of emergency airway event detection software integrated in the tracheostomy tube sensing accessory.